
AATOD...Follow Us 💫
National Organization Expanding Access to Quality Opioid Use Disorder Treatment Services Since 1984 #morethanmedicine #OUD
Statement for the Record
We are sharing AATOD's latest statement that corrects misleading testimony before the Senate Select Committee on Aging.
Get the details ➡️bit.ly/3DmpAvT⬅️
1 month ago
⏰THE CLOCK IS TICKING!
Please submit your proposals by tonight’s deadline - 3/4/25 at 11:59 PM EST.
SUBMIT ➡️ www.aatodconference.com
#aatod2025
#theevolvingfieldofopioidtreatment
1 month ago
⏰ TIME IS TICKING
The Call for Presentations Submission deadline is TOMORROW, March 4th.
Submit Presentation ➡️ aatodconference.com
This conference video message places a spotlight on AATOD's 2025 Workshop Committee Co-Chairs, Robert C. Lambert, MA, LADC & Allegra Schorr, MS. View their message and gain insight on what can be expected from the robust workshop lineup that is underway ➡️
https://bit.ly/3XpYwTa.
1 month ago
NEW Call for Presentations Submission Deadline: Tues, March 4, 2025
This week's video message places a spotlight on AATOD's 2025 Conference Chair, Joshua Nirella, MSOL. Click below to view as he formally invites each of you to attend this year's conference event, and calls for your personal involvement by submitting an abstract for a workshop or poster presentation.
https://youtu.be/EkSxR5j5GxI?si=ZSZvvzYHq1rVMBi3
#aatod2025
#theevolvingfieldofopioidtreatment
1 month ago
We are still accepting workshop proposals for the world’s premier training conference event for the treatment of Opioid Use Disorder.
#aatod2025
#TheEvolvingFieldofOpioidTreatment
Complete submission by this Tuesday, 3/4 ➡️ www.aatodconference.com
✍️ We need your help and expertise to achieve our conference goals.
1️⃣ Evaluate the rapidly changing nature and the severity of the opioid epidemic and associated outcomes and develop recommendations to improve the delivery of care in various populations based on evidence-based practices.
2️⃣ Interpret emerging trends and regulatory and policy changes to determine their effects on clinical practice.
3️⃣ Discuss peer support and peer-run programs in treating opioid use disorder to improve patient outcomes.
4️⃣ Review current evidence addressing the opioid epidemic and its implications for patients, clinicians, administrators, and policy makers by identifying the most effective interventions.
5️⃣ Disseminate innovative approaches, referral pathways, and partnerships designed to treat emerging needs of patients with opioid use disorder, address pivotal issues in health, and improve patient outcomes by providing examples of effective methods and how to implement them.
1 month ago
Newsflash!
Call for Presentations EXTENDED Submission Deadline:
📆 Tuesday, March 4, 2025
📣 We are pleased to announce that the deadline for submitting presentations has been extended to Tuesday, March 4, 2025. We encourage all interested parties to take advantage of this opportunity and submit proposals as soon as possible. We look forward to receiving your proposals and to seeing you in Philadelphia this October.
To submit a proposal, please visit our conference website,https://lnkd.in/e-Xr9vQv, and follow the on-screen instructions.
For questions or additional information, please send an email to info@aatod.org or call 856-423-3091.
#aatod2025
#theevolvingfieldofopioidtreatment
2 months ago
View the first of a series of #aatod2025 Conference videos which will feature messages from our Conference Committee Chairs throughout the conference planning stages and leading up to the AATOD Conference. This week's video message spotlights AATOD's President, Mark W. Parrino, MPA, as he highlights the significance of the conference theme and provides an update on the progress of our conference planning.
💻 bit.ly/3Q4HB4s
Call for Presentations Submission Deadline: February 25, 2025�
The world's premier training conference event for the treatment of Opioid Use Disorder.
#aatod2025
#TheEvolvingFieldofOpioidTreatment
2 months ago
📣 A Call for Presentations
#aatod2025
#TheEvolvingFieldofOpioidTreatment.
💻 To submit a proposal, please visit our conference website, aatodconference.com and follow the on-screen instructions.
✍️ We are encouraging a broad number of topics for submission in order to provide a rich learning content cutting across multiple disciplines to advance the work of our field. We expect nothing less than to continue to provide the most cutting edge information at the conference. Please join leading experts in the field and consider submitting a proposal highlighting your expertise in research or in the provision of care.
📅 Submission Deadline: Tuesday, February 25, 2025
2 months ago
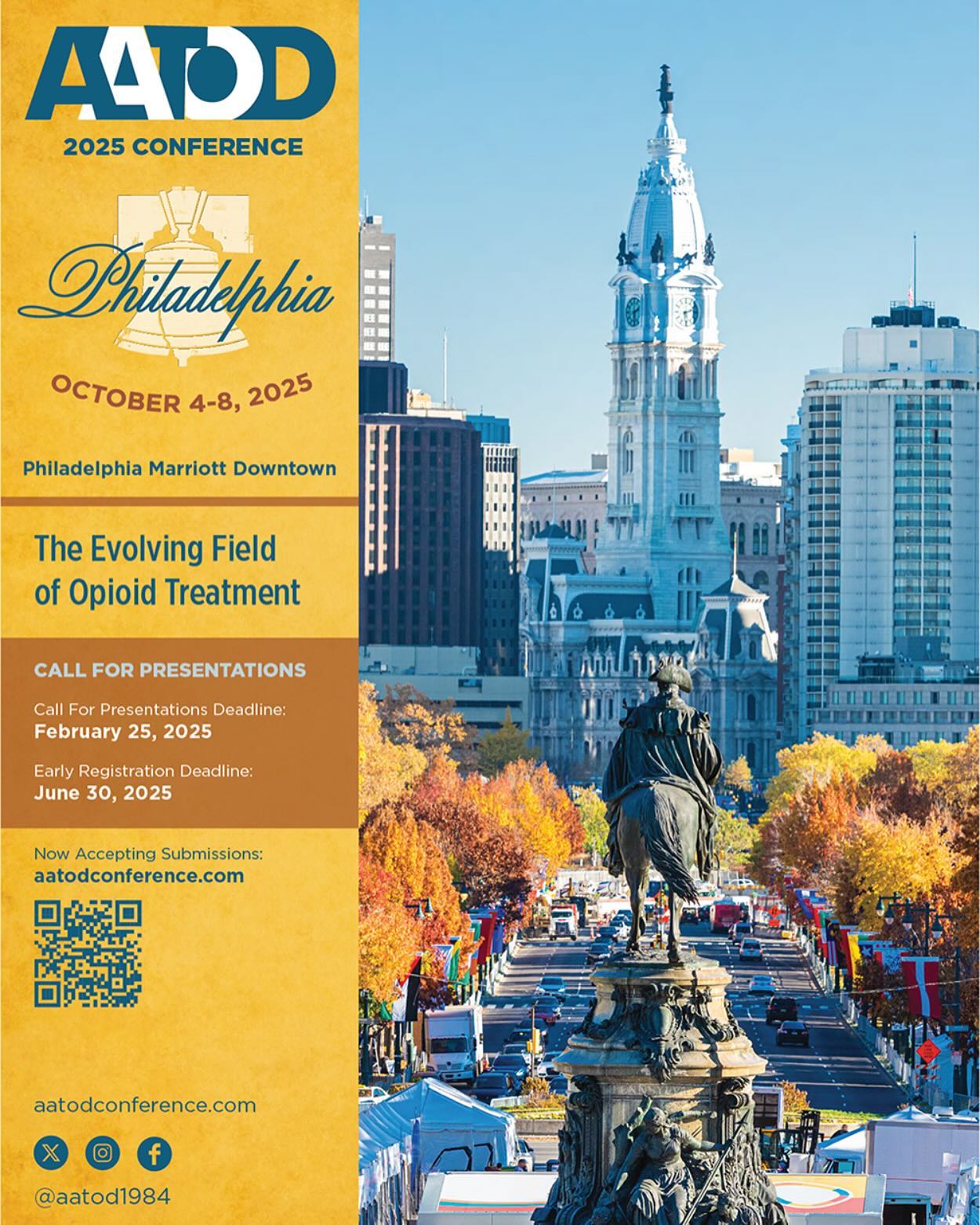
We’re Excited to Present the Official
AATOD Conference Announcement - #aatod2025 #theevolvingfieldofopioidtreatment
#savethedate
For more details ➡️aatodconference.com⬅️
3 months ago












RELEASED: AATOD State Chapter Responses on Mobile Vans 📘
➡️bit.ly/3BnJqGa⬅️
This report provides an overview of the barriers that OTPS have faced in expanding access to mobile van services in the United States. This includes the lack of Medicaid reimbursement for the services offered through such vans in addition to such state regulations and the need for sustainable funding sources.
It is our hope that this report will provide further guidance to OTPs in addition to federal and state officials. Our association has always taken the position that the use of mobile van services and non mobile medication units will increase access to the treatment of opioid use disorder in a meaningful and responsible way.
We continue to be grateful to the Opioid Response Network, the American Academy of Addiction Psychiatry (AAAP) and particularly the Substance Abuse and Mental Health Services Administration for their unwavering support in developing this project.
4 months ago
The Evolving Field of Opioid Treatment
AATOD proudly presents the world’s premier training conference event for the treatment of Opioid Use Disorder.
Early Registration Deadline: June 30, 2025
Visit www.aatodconference.com
#aatod2025 Conference Countdown
AATOD, Inc.
225 Varick Street, Suite 402
New York, New York 10014
Contact Us
Phone
: 212-566-5555
Email
: info@aatod.org
Social Sharing
OPIOID EDUCATION
Stay Connected to AATOD














